Health in Post-Conflict and Fragile States
Civilian health, health care workers, and health facilities disproportionately suffer in countries experiencing severe instability, but global health donors have yet to make developing health systems in such states a priority. Doing so could both make populations healthier and contribute to state legitimacy.

Summary
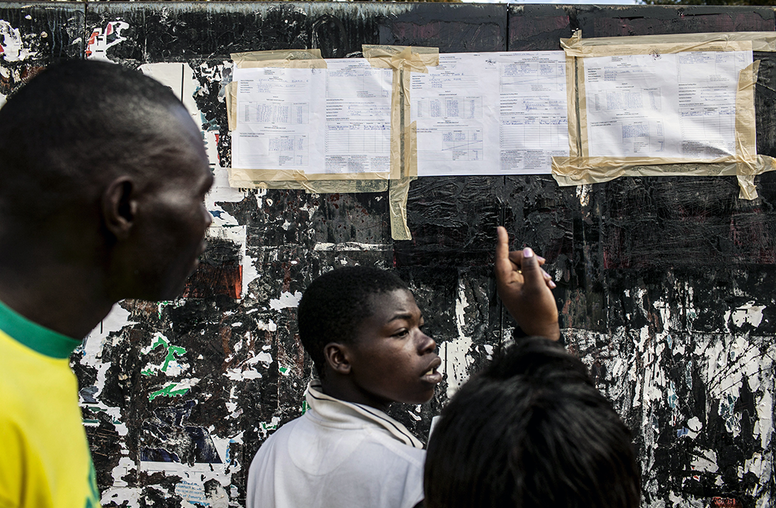
- The populations of states experiencing severe instability or unable to meet the basic functions of governance—referred to as fragile states—as well as those embroiled in conflict make up one-sixth of the world’s population and suffer from far poorer health than their counterparts in other states at comparable stages of development.
- During many armed conflicts, health facilities and health workers come under attack, and infrastructure is often destroyed, inducing health workers to leave and undermining management capacity, thus further depleting health system competence to meet basic needs.
- Evidence is emerging that effective and equitable health services may be a central contributor to state legitimacy.
- All too often, health interventions in fragile and conflict-affected states are limited to humanitarian relief, which does not advance either health systems development or state legitimacy.
- Two decades of experience in development of health systems in fragile and conflict-affected states have shown a need to address weaknesses in policy, leadership, management capacity, human resources for health, supplies, service delivery, and data collection and evaluation through World Health Organization’s (WHO) building blocks for health services.
- The military’s record of engagement in civilian health systems development is poor, and its efforts to use health interventions to promote stability have not proven fruitful. Its most appropriate role in civilian health in fragile and conflict-affected states is to provide or support health services in highly insecure areas.
- Donors have not made health systems development in such states a priority in global health programs. Investments are often seen as politically or financially risky, and as having lower potential payoffs. Given the poor health indicators in these states, however, health development in fragile and conflict-affected states should be a higher priority.
- Donors need to confront directly whether the goal of health development is stabilization or population health.
- Research is warranted on the relationships between health and armed conflict and between health development and state building.
About the Report
Because of the uncertainties and questions about health development in fragile and conflict-affected states, home to one-sixth of the world’s population, including whether and how it can advance state legitimacy or security, the United States Institute of Peace convened a two-day conference in June 2011—“Postconflict and Fragile States: Challenges for the Next Decade”—that brought together policymakers, organizations engaged in health development, ministries of health, human rights experts, academic researchers, and advocates to consider the questions and recommend a way forward. This Special Report is a product of that conference.
About the Authors
Rohini Jonnalagadda Haar is a physician who has engaged in clinical services, program development, and public health research in numerous countries with a variety of organizations. Leonard Rubenstein is a senior scholar at the Center for Public Health and Human Rights at the Johns Hopkins Bloomberg School of Public Health.
Guidelines for Use & Dissemination: You may download and print individual copies of this publication for your personal use. Permission requests for educational course packets are handled through Copyright Clearance Center www.copyright.com. All other perm